Authors: Meagan Chambers MD & Tanner Bartholow
Background
Gas embolism, a critical medical condition, occurs when gas bubbles enter the bloodstream and obstruct blood flow. These emboli most commonly arise from rapid changes in pressure, such as with scuba diving, invasive medical procedures, or trauma, allowing air or other gasses to enter the circulatory system. The consequences of gas emboli can be severe, ranging from organ dysfunction to potentially fatal blockages in vital arteries.
Quick Tips at Time of Autopsy
Clinical History
- Venous air emboli are most commonly caused by blunt head trauma or penetrating chest/neck trauma, thoracentesis, arterial catheterization, neurosurgery, or cardiac surgery. Of note, however, it may be considered in the differential of many sudden intraoperative deaths without an alternative or definitive explanation.
Internal examination
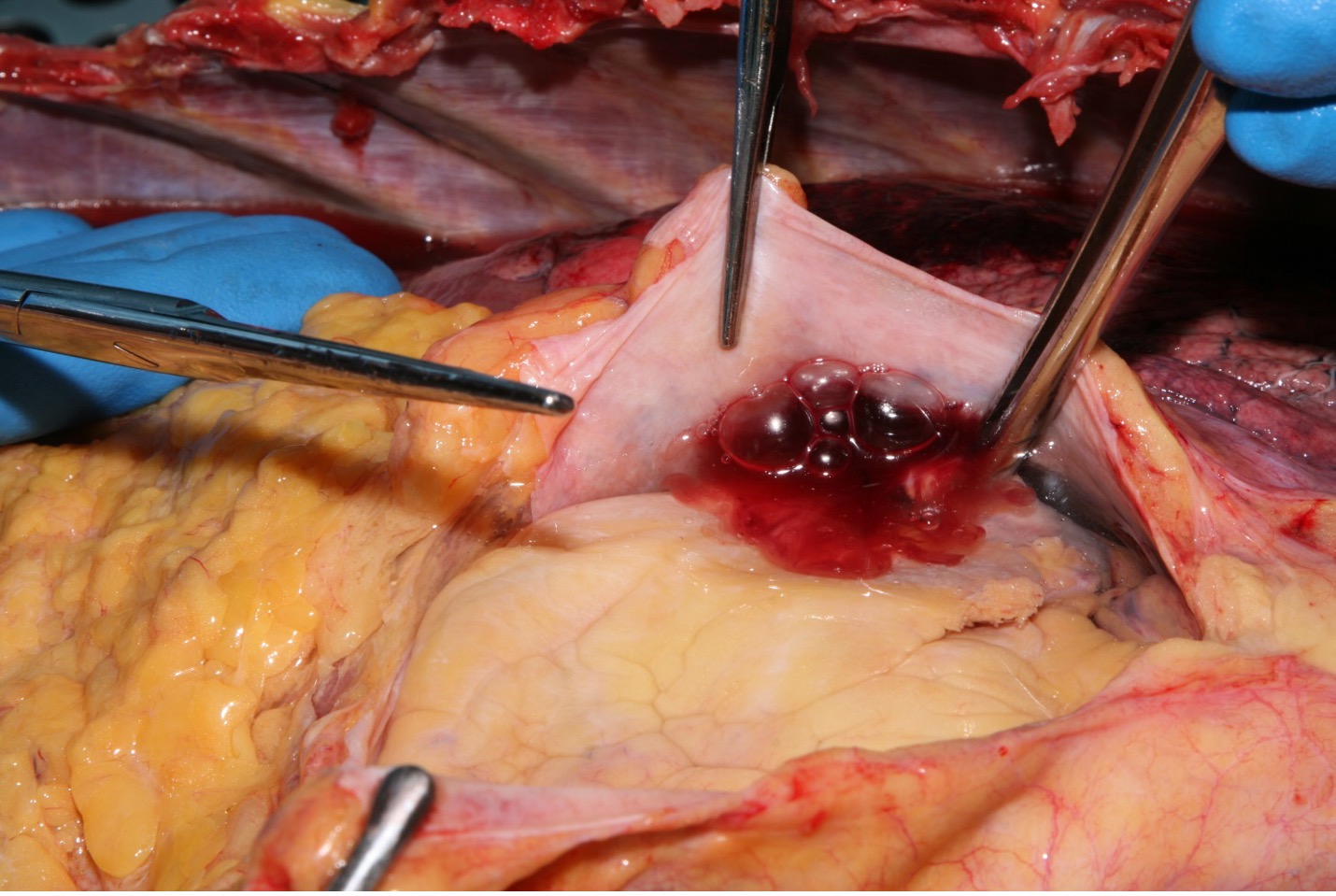
- In order to diagnose a venous air embolism in suspected cases, the manubrium and upper ribs are preserved in order not to damage the main vessels, and the remaining parts of the sternum and ribs are dissected carefully. The pericardium is punctured and filled with water. The right and left ventricles are penetrated underwater, and the presence of air bubbles is assessed (Petekkaya 2019).
 Image: Example of bubbles visualized in the setting of a gas embolus. (Image credit: Alex Williamson MD)
Image: Example of bubbles visualized in the setting of a gas embolus. (Image credit: Alex Williamson MD)
- Another method to diagnose an air embolism is to use a needle and 10ml syringe filled 50% with water to puncture the chambers and observe bubbles in the syringe during aspiration
- Of note, false positives can be seen in cases with longer postmortem intervals due to gas formation associated with putrefaction.
- Alternatively, there is a more complex procedure described by Bajanowski et. al which requires an aspirometer and analysis by gas chromatography.
- Frothy blood in the right ventricle also supports, but is not sufficient for the diagnosis.
- Post-mortem imaging (such as a simple chest X-ray) may be utility in these cases. This is especially true in cases of known penetrating/sharp force trauma, and may help explain the mechanism of death, in cases where insufficient trauma to explain the death is discovered at autopsy. Moreover, this is useful if cardiac valve recovery is taking place prior to autopsy, which, even with a subsequent complete cardiac examination, will result in a missed diagnosis.
Clinical Tidbits
- Venous air emboli occur in up to 76% of neurosurgical posterior fossa craniotomies, although the rate of a fatal embolism is much lower. Lower fatality is due to the rigid structure of the dural sinuses which do not collapse as other vessels do.
- During surgery, a sudden decrease in the end tidal CO2 volume and arterial oxygen saturation are important markers of an air embolism.
Recommended References
- Petekkaya S, Celbiş O, Oner BS, Turan Ö, Yener Z. A rare case of fatal venous and cerebral air embolism. Ulus Travma Acil Cerrahi Derg. 2019 May;25(3):311-315. English. doi: 10.5505/tjtes.2018.58201. PMID: 31135947.
Additional Citations:
- Bajanowski T, West A, Brinkmann B. Proof of fatal air embolism. Int J Legal Med. 1998;111(4):208-11. doi: 10.1007/s004140050153. PMID: 9646167.











One Comment