Authors: Alex K Williamson MD & Meagan Chambers MD
Background
Coronary artery bypass graft (CABG) surgery is performed for the treatment of coronary artery atherosclerosis. Evaluation of CABG interventions is an important component of postmortem evaluation of the cardiovascular system.
There are two types of CABG procedure
- Internal mammary artery (IMA) graft, wherein an IMA is transected and its distal end is then sutured into a coronary artery distal to that artery’s site of stenosis, forming the “distal anastomosis”
- Saphenous vein graft, wherein a segment of saphenous vein is harvested from the leg and one end is then sutured into the ascending aorta, forming the “proximal anastomosis”, and the other end is sutured into a coronary artery distal to the artery’s site of stenosis, forming the “distal anastomosis”
- A radial artery graft, where in a segment of the radial artery is harvested from the forearm and one end is then sutured into the ascending aorta, forming the proximal anastomosis, and the other end is sutured into a coronary artery distal to the artery’s site of stenosis, forming the distal anastomosis.
 (Image Credit: Mayo Clinic)
(Image Credit: Mayo Clinic)
- A person may have had one or more CABG procedures at one or more points in time, and one or more types of CABG surgery/grafts may have been employed in surgical management of atherosclerotic heart disease.
Quick Tips at Time of Autopsy
Clinical History
- The terms “triple” or “quadruple” bypass refer to the number of target vessel anastomoses (i.e., the number of vessels that are bypassed), rather than the number of graft conduits
External examination
- Clues to the presence of CABG surgery on external examination include a midline sternal scar and a scar on the medial lower extremity(ies) in the vicinity of the saphenous vein(s)
 Image: Leg scar from harvesting graft tissue for CABG. (Image credit: Doctor’s Hub).
Image: Leg scar from harvesting graft tissue for CABG. (Image credit: Doctor’s Hub).
 Image: Increasingly, arteries are procured laparoscopically, with smaller surgical incisions. This patient passed within 2 weeks of his CABG procedure and therefore the incision is still fresh with associated erythema and ecchymosis. (Image credit: Meagan Chambers/Stanford Hospital).
Image: Increasingly, arteries are procured laparoscopically, with smaller surgical incisions. This patient passed within 2 weeks of his CABG procedure and therefore the incision is still fresh with associated erythema and ecchymosis. (Image credit: Meagan Chambers/Stanford Hospital).
Internal examination
- IMA grafts should be identified at the time of removing the chest plate during dissection. Their proximal ends will have to be transected as the chest plate is removed. Clamping any definitive or suspected IMA at the time of chest plate removal facilitates IMA identification and evaluation during subsequent heart examination
- The heart can be dissected from the organ block in the usual fashion. If there is no ascending aorta pathology then the heart including proximal great vessels can be removed from the chest block in the usual fashion, leaving about 4.0 cm of ascending aorta attached to the heart
- Remove fibrous tissue and residual pericardium from the around the heart by carefully lysing all adhesions in order to reveal the epicardial surface, native coronary arteries, and bypass grafts. Keep all dissected tissues handy in case they include part(s) of a CABG that were inadvertently excised
- Make two longitudinal incisions, one along each lateral aspect of the ascending aorta, to form a “clam shell” with anterior and posterior flaps of the ascending aorta. Visualize the aortic valve cusps, sinuses of Valsalva, and native coronary artery ostia. Document any graft attachment sites

Image: Aortic valve with two graft insertion points with associated sutures. (Image credit: Meagan Chambers/University of Washington)
- Identify any proximal aortocoronary artery bypass graft ostia, which will almost always reside in the anterior ascending aorta, about 2-3 cm above the aortic valve. These ostia are characterized by small round defects, with diameters similar to those of the native coronary artery ostia, which are surrounded by sutures. Gentle probing can be used to differentiate patent from closed ostia, as well as to determine angle of take-off from the aorta, but deep and vigorous probing should be avoided as it can dislodge potentially pathologic atherosclerotic plaque and/or thrombus
- Note that in order to perform any CABG surgery, the heart had to be placed on cardiopulmonary bypass, and so there will almost always be a healed defect in the anterior ascending aorta, probably containing one or more sutures, which represents the cannulation site for cardiopulmonary bypass. This is not a proximal aortocoronary bypass anastomosis
- Trace all bypass graft vessels from either 1) their proximal anastomosis origin on the aorta or 2) as an internal mammary artery to their distal anastomosis site on an affected coronary artery. Evaluate the integrity of any proximal and distal anastomoses as well as the palpable pliability of the bypass vessels
- Remove the three native epicardial coronary arteries in the usual fashion. Ideally, each bypass graft will be taken off and kept in distal continuity with the native coronary artery it serves. In cases of aortocoronary artery bypass grafts, the proximal end of the graft vessel can be transected just distal to the proximal aortocoronary anastomosis. In cases of IMA grafts the vessel will already be mobilized for removal with the native coronary artery it serves (usually the LAD)

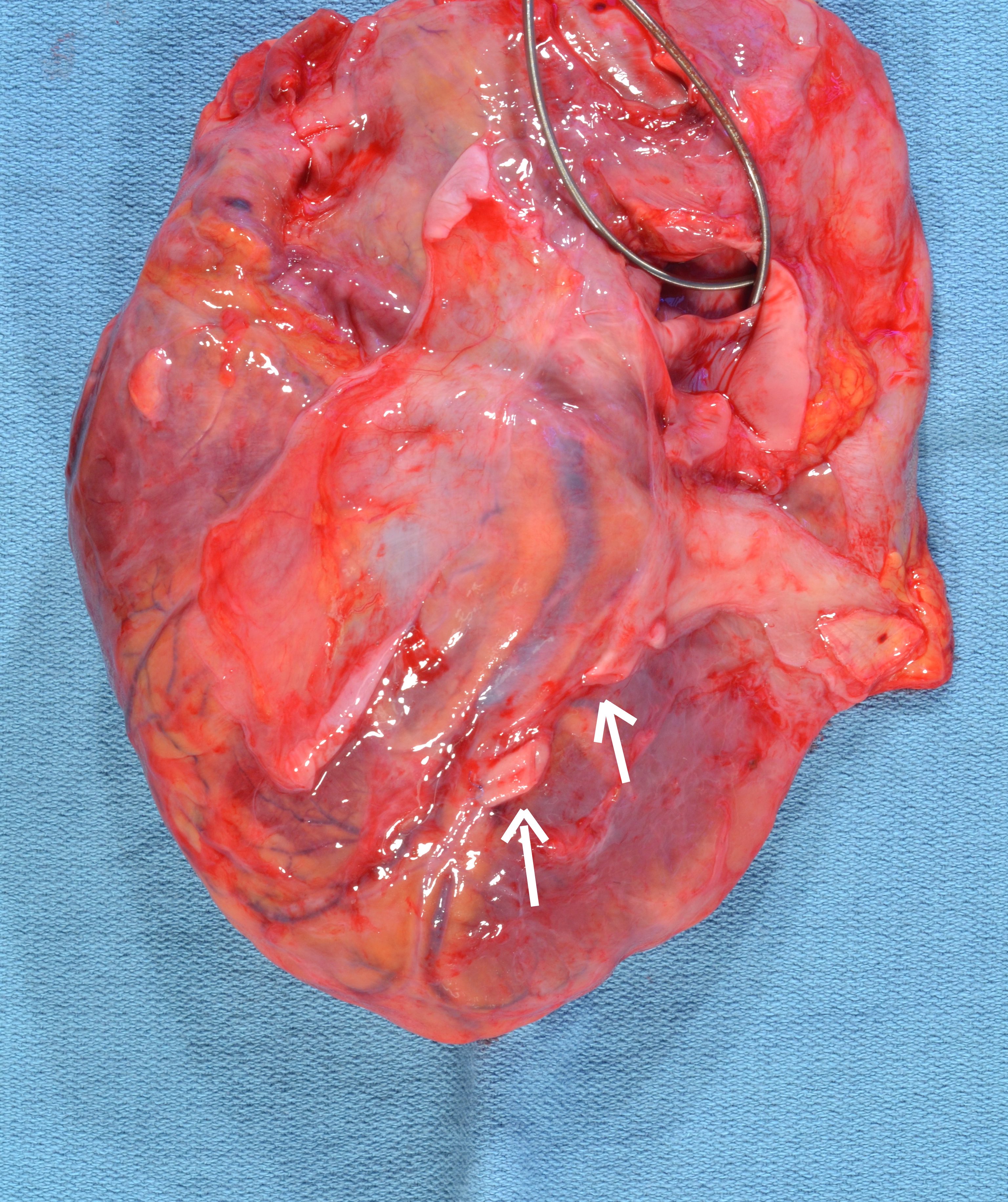
IMAGE: Anterior view of autopsied heart shows aortocoronary saphenous vein grafts to right coronary (thin black arrow), left anterior descending (LAD) (fat white arrow), and obtuse marginal (thin white curved arrow) targets. An additional posterior descending graft (thin white straight arrow) has been cut. (Image credit: Dylan Miller via ExpertPath)
 Image: On fresh examination, this quadruple bypass has a left internal mammary to LAD graft (black arrows), radial artery from aorta to left marginal and diagonal arteries (yellows arrows), and saphenous artery from aorta to posterior descending artery (blue arrows). (Image credit: Meagan Chambers/Stanford Hospital)
Image: On fresh examination, this quadruple bypass has a left internal mammary to LAD graft (black arrows), radial artery from aorta to left marginal and diagonal arteries (yellows arrows), and saphenous artery from aorta to posterior descending artery (blue arrows). (Image credit: Meagan Chambers/Stanford Hospital)
- Sections to submit for histology: Fix, decalcify as appropriate, and serially section the native coronary arteries and graft vessels. Submit for histology the most stenotic regions of each native coronary artery and any abnormal areas within each graft vessel. Sections of native coronary artery (e.g., 3 most stenotic sections) and sections of the graft vessel to that vessel (e.g., 3 sections showing pathology, or randomly selected section) can be submitted in one cassette for each artery. One should become familiar with atherosclerosis in native vessels, arterialization of venous graft vessels, and atherosclerosis in graft vessels
Click here for examples of Gross Descriptions
Ancillary testing:
- If stents are present, they should be visually inspected for a thrombus. If light does not pass through the lumen then the specimen can be sent for consultation to a laboratory for laser cutting which will allow the thrombus to be viewed histologically in relation to the stent.
- As the anatomic landmarks for hearts with prior surgeries are harder to identify due to scarring and fibrosis, an x-ray of the heart at the time of gross dissection can be helpful in identifying the location of metal stents
 Image: This heart (seen grossly on the left and by x-ray on the right) is a combination of metal stents and CABGs. The metal stents can be easily visualized by x-ray. (Image credit: Meagan Chambers/University of Washington).
Image: This heart (seen grossly on the left and by x-ray on the right) is a combination of metal stents and CABGs. The metal stents can be easily visualized by x-ray. (Image credit: Meagan Chambers/University of Washington).
Quick Tips at Time of Histology Evaluation
- Evaluate sections for plaques, thrombosis, recanalization, etc. Reporting a % stenosis can be done grossly or microscopically
- The internal mammary artery graft has a characteristic multi laminar elastic artery wall with concentric layers of elastic fibers within the media (as visualized on VVG or similar special stain) while other arterial grafts such as the saphernous or radial artery will have a single internal elastic lamina
 Image: Internal mammary artery with characteristic multi-layered elastic lamina on EVG staining. (Image credit: Meagan Chambers/Stanford Hospital)
Image: Internal mammary artery with characteristic multi-layered elastic lamina on EVG staining. (Image credit: Meagan Chambers/Stanford Hospital)
 Image: Radial artery with single internal elastic lamina and single external elastic lamina on EVG staining. (Image credit: Meagan Chambers/Stanford Hospital)
Image: Radial artery with single internal elastic lamina and single external elastic lamina on EVG staining. (Image credit: Meagan Chambers/Stanford Hospital)
- Venous grafts have a single elastic lamina and adventitial smooth muscle bundles. Arterialization can cause a distinct internal elastic lamina, intimal fibroplasia, and plaques
 Image: Saphenous vein graft with single external elastic lamina, and no/faint internal elastic lamina on EVG staining. (Image credit: Meagan Chambers/Stanford Hospital)
Image: Saphenous vein graft with single external elastic lamina, and no/faint internal elastic lamina on EVG staining. (Image credit: Meagan Chambers/Stanford Hospital)
- The anastomosis will have a “figure 8” composed of partial lumens from the native and graft vessels. Paired suture holes can be useful landmarks (“snake eyes”)
 Image: Internal mammary artery graft (left side of image) anastomosis with distal LAD (right side of image). Embedded sutures are seen at the anastomosis (“snake eyes”), as well as atherosclerotic changes in the native LAD. (Image credit: Meagan Chambers/Stanford Hospital).
Image: Internal mammary artery graft (left side of image) anastomosis with distal LAD (right side of image). Embedded sutures are seen at the anastomosis (“snake eyes”), as well as atherosclerotic changes in the native LAD. (Image credit: Meagan Chambers/Stanford Hospital).
- Guidewire emboli can be seen in small to medium sized vessels in some cases following percutaneous coronary stenting
Quick Tips at Time of Reporting
- The convention for CABG labeling is to hyphenate the target vessel first, then the graft vessel (LAD-D1-LIMA would be a left internal mammary graft to the 1st diagonal branch of the LAD)
Click here for examples of incorporating CABG findings into the autopsy report
Clinical Tidbits
- 90% of internal mammary artery grafts are patent at 10 years, while only 20-30% of saphenous vein grafts are patent at 10 years
- Early complications include kinking or acute thrombosis (secondary to hypercoagulability). Late complications include fibrointimal proliferation and atheromatous plaques
- CABG has largely been replaced by stenting and other less invasive procedures, but it is still done in cases of multiple heart pathologies requiring open heart surgery (such as valve replacement and coronary artery disease), left main coronary disease (due to higher rates of complications), and multifocal vessel disease

Image: Guidewire emboli appear as basophilic granular/serpiginous material in vessel lumen. (Image credit: Meagan Chambers/University of Washington).
Recommended References
- Lee AH, Gallagher PJ. Post-mortem examination after cardiac surgery. Histopathology. 1998 Nov;33(5):399-405. doi: 10.1046/j.1365-2559.1998.00570.x. PMID: 9839163.
Additional Citations:
- Miller, Dyllan. Coronary Artery Bypass Grafting. ExpertPath. Accessed 2023. (ExpertPath Login Required)
- Otsuka F, Yahagi K, Sakakura K, Virmani R. Why is the mammary artery so special and what protects it from atherosclerosis? Ann Cardiothorac Surg. 2013 Jul;2(4):519-26. doi: 10.3978/j.issn.2225-319X.2013.07.06. PMID: 23977631; PMCID: PMC3741888.
- Ruengsakulrach P, Sinclair R, Komeda M, Raman J, Gordon I, Buxton B. Comparative histopathology of radial artery versus internal thoracic artery and risk factors for development of intimal hyperplasia and atherosclerosis. Circulation. 1999 Nov 9;100(19 Suppl):II139-44. doi: 10.1161/01.cir.100.suppl_2.ii-139. PMID: 10567293.











One Comment